In Health Action International’s 40 years exploring and offering solutions to the eternal problem of weak health systems, we have never encountered a situation in which these weaknesses were so laid bare, or as damaging, as they have been during recent pandemics, such as Ebola and now COVID-19.
COVID-19 in particular has exposed weaknesses in almost all health systems, in countries both rich and poor. From within our team’s focus areas, known issues are being drawn into sharp focus, whilst additional problems are uncovered daily. This situation requires an agile advocacy response with our partners across the world, who are experiencing the consequences of a fragmented, and in some instances broken, health system.
Fortunately, our project teams and partners have a lot of experience in exposing, addressing, and advocating for change in weak health systems. This has meant that while we’ve had to pivot on occasion, we are in a strong position to advocate for access to medicines for everyone, everywhere.
This is an overview of the work each of our projects are focusing on at the moment, and the impact of COVID-19 on their areas of focus.
Research for ICEMs and Access to Medicines
Despite the COVID-19 restrictions, our research team in partnership with our interns have, through creative and flexible approaches, managed to collect valuable data. As travel and face-to-face meetings became impossible, all data was collected digitally. Amongst others, we interviewed a variety of Kenyan stakeholders on barriers to access Internationally Controlled Essential Medicines (ICEMs), analysed longitudinal data on the availability and affordability of sexual and reproductive health commodities in Kenya, Uganda and Zambia, and interviewed experts in the EU about European collaboration on Health Technology Assessments.
Access to ICEMs was problematic even before the pandemic, as these medicines have extensive regulatory requirements imposed on them in many countries. Of course, controlled medicines are by their nature subject to international treaty, but the overly rigorous interpretation of those rules and enthusiastic implementation cause massive barriers to access for those in need. Sadly, issues have only worsened due to disrupted supply chains, lock down measures and increased use of some ICEMs such as morphine in the care of COVID-19 patients which strains the supply chain. Morphine can relieve shortness of breath, serious pain and suffering related to COVID-19. While we currently lack reliable data on access and shortages in developing countries, countries such as France, the United Kingdom and the United States are already facing shortages of opioids, even though they, together with some other developed countries, have access to 90% of the opioids available worldwide.
In a published comment in the Lancet, experts, including the president of the International Narcotics Control Board (INCB), emphasised the key role palliative care and opioids play in the care of COVID-19 patients. In a separate statement the INCB also stressed to governments that they can make use of simplified procedures for the import and export of controlled medicines, and thus morphine, in times like these when they are sorely needed, and that governments should make use of this procedure to increase their national opioid reserves. However, the question remains, are governments equipped, both in capacity and human resources, to do this when they are already overburdened and overrun?

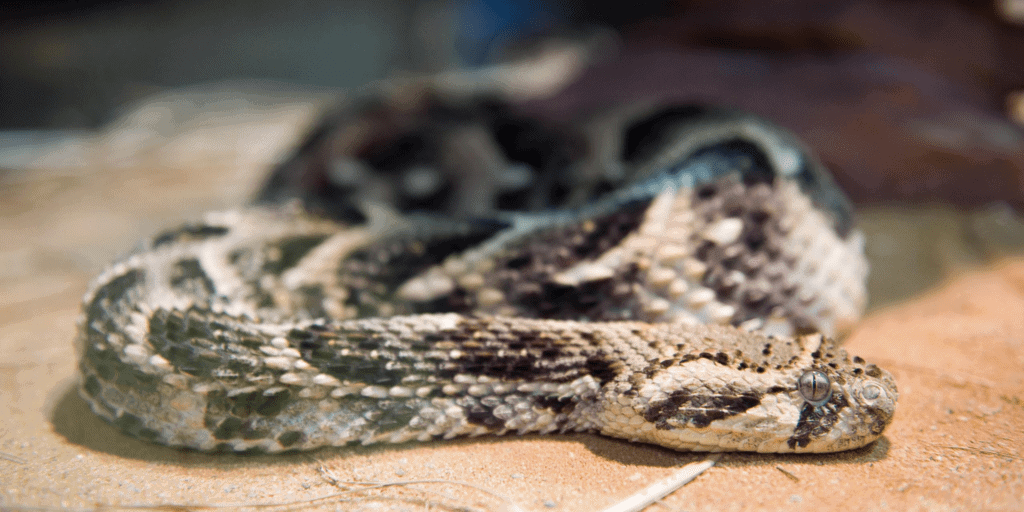
Snakebite
Snakebite, like other neglected tropical diseases (NTDs), knows no boundaries and continues to affect people’s lives during the COVID-19 pandemic. In some instances, civil society leaders are reporting even worse outcomes for individuals, further exposing the weaknesses in existing health systems that should be managing snakebites. Despite this, we continue to use our evidence-based research to inform health authorities on policies and tools that improve snakebite prevention, treatment and management responses through COVID-19 and beyond.
Field research in Kenya has again resumed after initial restrictions were lifted, and we have adapted our research tools to complement the authorities in response to COVID-19. Using our integral role in convening civil society and community actors, in July we hosted a first of its kind international webinar aimed at empowering the voices of women community actors responding to snakebite in the current landscape. We are again supporting the theme of ‘Women Champions of Snakebite’ by co-organising activities to support this year’s International Snakebite Awareness Day (ISBAD) 2020. We will continue to work toward supporting communities that are affected by fragile health systems that have been further compromised by COVID-19.
ACCISS study
Life in the time of COVID-19 has created additional problems for people living with diabetes. Studies have shown those with type 2 diabetes, and those with uncontrolled type 1 diabetes, are at risk of more severe cases of COVID- 19. Further, lockdowns, travel restrictions, economic uncertainty and an over-stretched health system can all impact diabetes care. Working with our partners, we are currently trying to understand how COVID is directly affecting people living with diabetes. Our partner CRONICAS in Peru, which is a country with a high COVID prevalence, is currently conducting an online survey of people living with type 1 diabetes to see what impact the virus is having on accessing insulin and care. While COVID-19 has uncovered weaknesses in health systems, it has also fortified our resolve to continue on the path we were on prior to the pandemic. For example, in Kyrgyzstan the management of type 1 diabetes is predominantly undertaken in the capital Bishkek. Under lockdown, where travel has been severely restricted, people living outside of Bishkek have been unable to travel for appointments with their endocrinologist. Prior to lockdown, our partner HPAC had started training family doctors on diabetes care in regions outside of the city to help ensure a continuum of care for people living with diabetes. Now, more than ever, this training must continue and expand to other health care workers after lockdown restrictions are over.
Other current work includes the pilot study in Mali of our new apps and dashboards for regular monitoring of the availability and prices of insulin, syringes, test strips, glucometers and other supplies. The first round of data collection in households has been completed, and data collection in public hospital clinics and private pharmacies is ongoing. We are looking forward to seeing the findings, especially from the households as the needs of insulin users is what we are trying to meet in the ACCISS Study. A key part of the current work of the ACCISS Study is preparing for next year’s centenary of the discovery of insulin. It is an important milestone to reflect on both the achievements of the last 100 years and also the gaps in access to insulin and care for all who need it. As part of this commemoration we are advocating for a World Health Assembly (WHA) resolution on access to insulin in 2021. In June, we co-hosted a webinar to discuss this proposal, bringing together key stakeholders in a panel discussion, and a discussion with an active audience of over 200 people. There was clear support for a resolution so it is hoped that it will be on the WHA 2021 agenda.
Looking ahead, we believe that the impact of COVID will be felt for years to come and in many different ways. For example, a recently released study has found a connection between COVID-19 and an increase in type 1 diabetes in children. We hope that the lessons learnt during this time, by us and by others, will build our understanding of the impact of the pandemic, and help strengthen health systems everywhere to improve their ability to care for people living with diabetes.

European Projects
The first half of 2020 has been challenging for the European Projects Team (EPT), as our planned activities, scheduled deadlines and even working conditions have been affected by the COVID-19 pandemic. In fact, the Coronavirus outbreak has laid bare the shortcomings of the current Research & Development model and the obstacles posed to access to medicines by the lack of transparency and misuse and abuse of intellectual property rules. This is now hindering the progress towards a vaccine or other therapeutic response to the pandemic.
The EPT has remained active at our usual three levels of action: national (Netherlands), regional (European Union) and global. We have engaged with a wide range of stakeholders such as policy makers, public officials, and industry representatives, and collaborated with fellow advocates and other public interest civil society organisations. We have also consolidated our networks at the European Parliament through the Working Group on Access to medicines, and continued to provide technical advice to the European Medicines Agency and contribute to discussions at the World Health Organization (WHO) around the COVID-19 resolution.
We have been able to frame our COVID-related work within our strategic plan of promoting access, ensuring transparency and ensuring sustainable innovation of medicines. Public events, such as the relaunch for a German audience of the report on socially sustainable licensing and access to medicines, have been successfully turned into webinars. We have led drafting efforts for joint letters, with civil society and MEPs, on the need for public return for public investments that have merited responses by the European Commission clarifying its position on accessibility clauses or sharing of data. Importantly, we remain committed to pursuing this dialogue. Additionally, we have responded to two relevant public consultations organised by the European Commission on the new pharma strategy roadmap and about the Intellectual Property Action plan (jointly with Wemos). As COVID-19 exposes weaknesses in health systems over the coming months, the EPT will continue to highlight these and advocate for greater transparency and collaboration so that a vaccine or therapeutic response can be accessed by everyone, everywhere.

HAI’s focus areas include:
Snakebite, Access to Insulin, Health Systems Advocacy Partnership, Medicines in Europe, Prices, Availability and Affordability