As the COVID-19 crisis continues to hold the world in its grip, more and more stories and prognoses are emerging about its impact on other aspects of life and health. Dorothy Okemo and Denis Kibira , HAI partners in the Health System Advocacy (HSA) Partnership, have written about the impact of COVID-19 on access to sexual and reproductive health (SRH) services in Kenya and Uganda, and similar stories continue to come out on a daily basis across sub-Saharan Africa. The United Nations Population Fund (UNFPA) estimates that the impact on SRH will be devastating. They project that if lockdowns last for six months or longer:
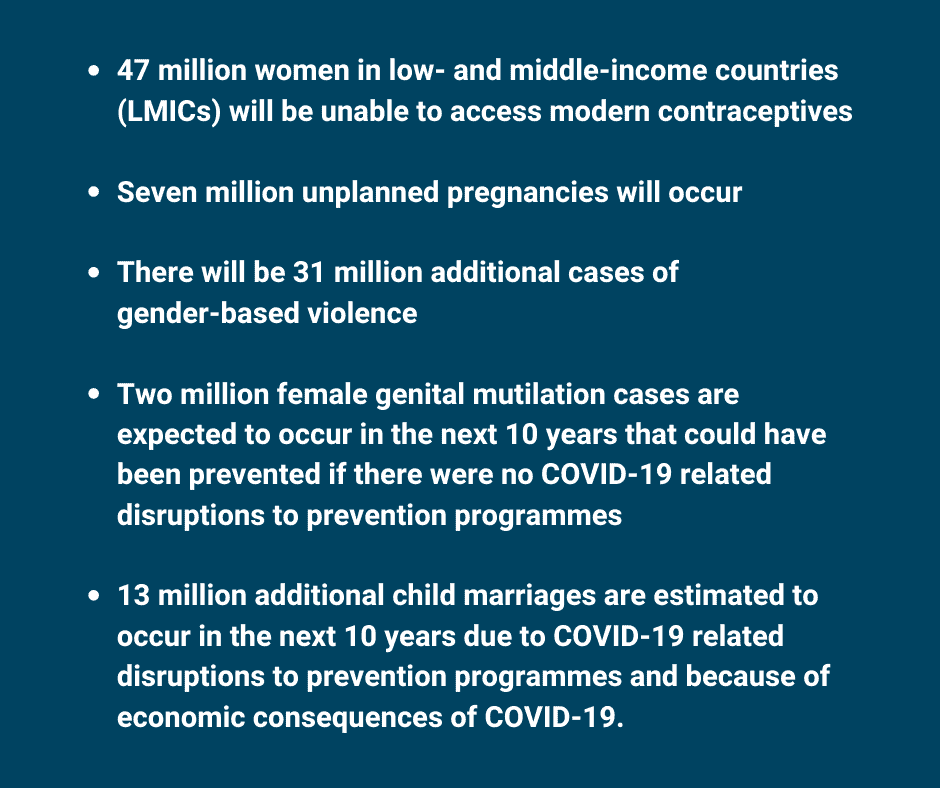
Understanding the additional crisis that lack of access to SRH would cause, especially in LMICs, 59 governments have underscored the necessity of ensuring continued provision of SRH services to prevent a rise in avoidable, unmet family planning needs, sexually transmitted infections, unsafe abortions, and maternal and newborn deaths.
COVID-19 not only impacts the SRH of girls and women, it also has far-reaching consequences for the rest of the health system in many countries. As Director General of the World Health Organization (WHO) Dr. Tedros remarked recently:
As the pandemic has spread, its public health and socioeconomic impacts have been profound, and have disproportionately affected the vulnerable. Many populations have already experienced a lack of access to routine, essential health services.
In sub-Saharan Africa, access to essential interventions is already being compromised. Case in point is that in Chad, Ethiopia, Nigeria and South Sudan, disruptions in measle vaccination programmes have left over 20 million children unprotected. Gavi, the vaccine alliance, has postponed 14 vaccination programmes against polio, measles, cholera, human papillomavirus, yellow fever and meningitis, which would have covered over 13 million people. The WHO has also made the decision to redirect resources meant for the vaccination of 12 million children in sub-Saharan Africa against polio to COVID-19. The WHO further warned that deaths caused by malaria could increase to more than 700,000 in sub-Saharan Africa this year if prevention and treatment programmes are disrupted by COVID-19. As the Bill & Melinda Gates Foundation has pledged to shift almost its entire organisation to focus on COVID-19, what will it mean for their programmes on HIV, malaria and polio eradication, especially now when those type of programmes are already suffering from COVID-19 related disruptions? What these cases expose is what some would call the systemic problem of over-reliance on donor aid for provision of essential health interventions in many LMICs. With these donor-funded programmes falling away, the gaps in LMICs’ own capacity to provide these services are revealed.
So, as the world reacts to the COVID-19 crisis and pledges billions of dollars to tackle this pandemic, it is more important than ever to conceptualise health holistically, taking into account its social and economic determinants as it is the forthcoming economic and food crises that will also drastically impact public health and health service provision in LMICs, perhaps even more than COVID-19 ever would. In their approaches to dealing with COVID-19, national governments and aid agencies must ensure that continued access to essential health services is on their agenda, and that measures are taken to mitigate the impact of the economic consequences of the pandemic felt by many. If not, we are likely to be facing an additional health crisis in LMICs in the very near future, which will reverse years of development.