A simple complication during pregnancy can lead to devastating consequences for Ugandan families.
Preeclampsia affects between 2-8% of pregnant women worldwide. For Ugandan women however, a diagnosis of preeclampsia could result in becoming one of the many preventable deaths caused by pregnancy-related complications.
Preeclampsia is characterised by high blood pressure and damage to organs. If not managed, it can lead to slower growth of the fetus, preterm birth, organ damage, and eclampsia, which results in the expectant mother experiencing seizures.
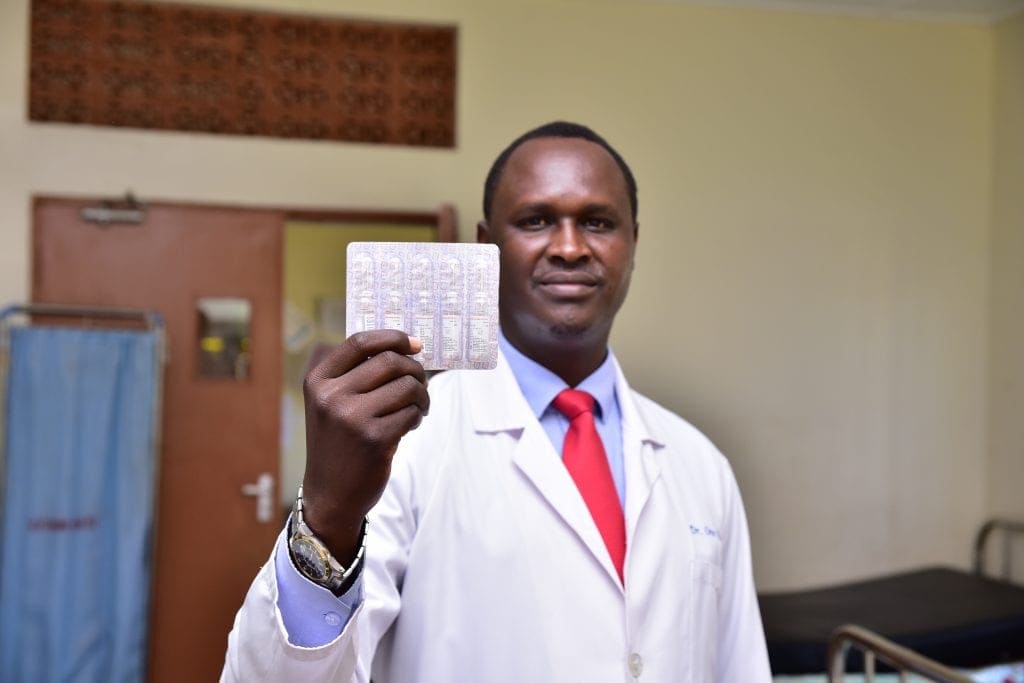
“Pre-eclampsia is a deadly condition that can damage a woman’s vital body organs such as the liver, kidney, brain and the blood system. If not managed properly, both the woman and the unborn baby can die. That is why we need sustainable interventions for proper management of the condition” – Dr. Isaac Orec, the In-charge at Amach Health Center IV.

Dr. Isaac Orec, the In-charge at Amach Health Center IV.
Magnesium sulphate and dexamethasone can be used to manage the condition, but frequent stock outs mean it isn’t always available to women in Ugandan Health Centres, such as Lira Referral Hospital and Amach Health Center IV.
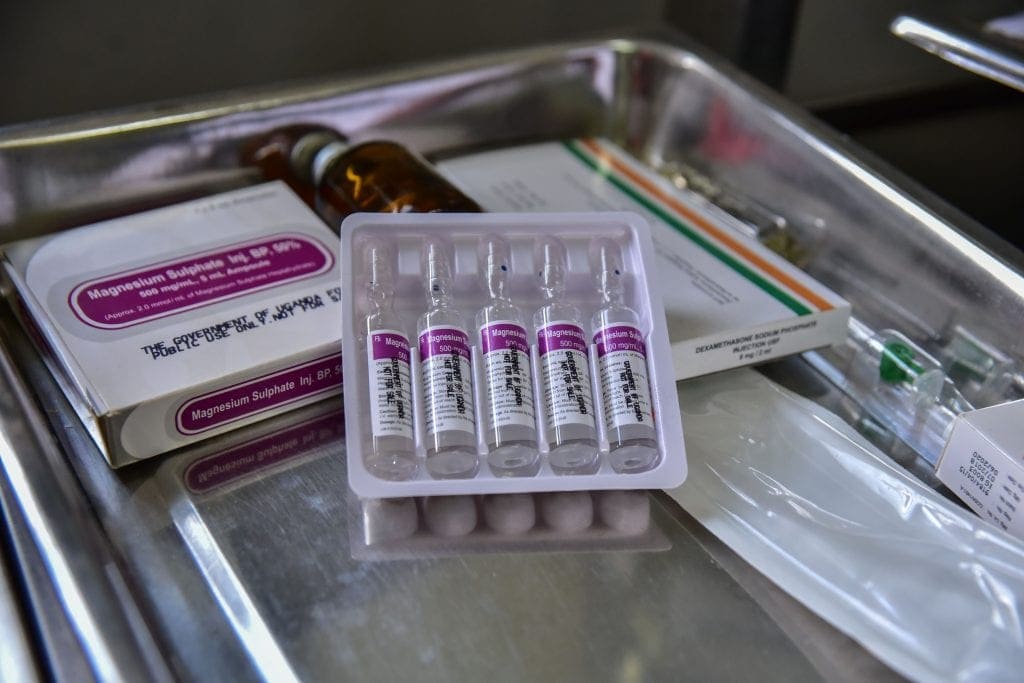
Magnesium sulphate.

Lira Referral Hospital.
Our partners at HEPS Uganda, working with HAI as part of the Health Systems Advocacy (HSA) Partnership, are fighting this devastating condition by raising awareness and advocating for policies that can lead to better care for women suffering from preeclampsia.
One of the first steps in their journey was organising a media orientation about the condition, along with a community visit so the media could see firsthand the terrible toll preeclampsia can take, and how it can be avoided.
With an increase in media attention, Members of Parliament (MPs) and politicians started to take notice. Policy makers were taken for a field visit in Kawempe Hospital to further emphasise the implications of lack of medicines for Ugandan women and families.
With this momentum, MPs presented a paper on the floor of Parliament highlighting the challenges that Kawempe Hospital encounters in managing mothers with preeclampsia. The challenges included, frequent stock-outs of essential medicines, such as magnesium sulphate, lack of oxygen cylinders, incubators, among others.

The Speaker of Parliament, Rt. Hon. Rebecca Alitwala Kadaga, signing a commitment board pledging to support funding for magnesium sulphate.
The Speaker of the Parliament took notice and directed the Ministry of Health to conduct investigations into this previously overlooked issue. In addition to this, increased funding for magnesium sulphate was provided.

Members of Parliament sign commitment board pledging to become champions and advocates of better management of preeclampsia.
“Community engagement was very key in our preeclampsia advocacy and it is amazing to see how communities took up the issue with passion.
For example, in Lira district we started with a symposium where we sensitised the public about the condition and the response was positive. We see community leaders coming up to become champions of preeclampsia.” – Ms. Jackie Mutimba, Assistant coordinator HSAP- HEPS Uganda.
These outcomes have been incredibly exciting for the HSA Partnership. It has demonstrated the power of building partnerships with communities, local civil society, and national and international private and public actors to create meaningful, tangible change.
But far more importantly, it has meant that women diagnosed with preeclampsia may no longer have to become a statistic of the thousands of pregnancy-related deaths.
“I lost my first born due to preeclampsia condition because I was naïve and did not go to a hospital when my feet started swelling. People told me that the swelling of the legs was a sign of twins.” Mrs Mary Odongo (pictured below).
“But for my second pregnancy, I came in immediately I discovered I was pregnant and the doctors have been helpful.”

“I lost my first born due to preeclampsia condition… for my second pregnancy, I came in immediately I discovered I was pregnant and the doctors have been helpful.” Mrs Mary Odongo (pictured, right).
Image credits: Nicholas Bamulanzeki and HEPS Uganda.