by BOBBI KLETTKE
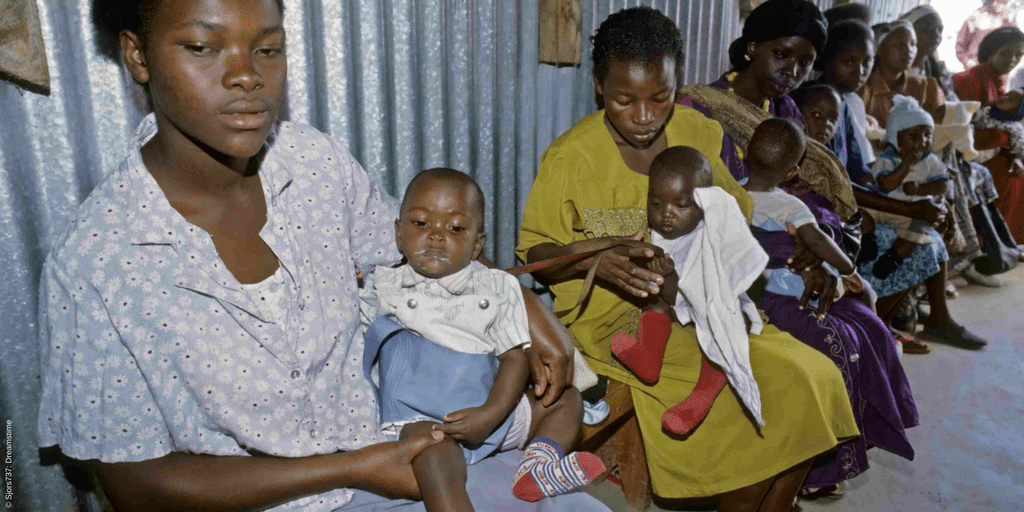
When 21-year-old Kissa Ojok became pregnant with her first child, she feared for her life. For years, she had heard stories from other women in her community, a rural village in central Uganda, about the pain, suffering—even death—that many before her had endured during pregnancy and childbirth. She had also heard, first hand, the horrors that many mothers faced in losing their newborn babies.
Kissa’s fears were well warranted. Every year in sub-Saharan Africa, there are approximately 289,000 cases of maternal mortality—the highest rate in the world. For every woman who dies, about 20 others suffer serious injuries, infections, or disabilities. And despite a decline in the under-five child mortality rate since 2000, the risk of death in the first month is still greatest in sub-Saharan countries.
These daunting statistics have long been of interest to Health Action International’s (HAI) senior research manager, Dr Gemma Buckland-Merrett. Knowing that these deaths could partly be prevented with adequate access to essential medicines and supplies, she devised a five-year study to measure the price, availability and affordability of sexual and reproductive health commodities in public, private and mission healthcare facilities throughout Kenya, Uganda and Zambia.
“There’s a tremendous amount of anecdotal information about the lack of essential medicines and devices for sexual and reproductive health,” says Gemma. “But governments need robust data to develop and implement strong policies to improve the sexual and reproductive health of citizens.”
Gemma designed the study using the gold-standard methodology developed by HAI and the World Health Organization (WHO). Working with Denis Kibira, director of the Kampala-based health campaigning organisation, HEPS Uganda, she went on to identify more than 30 sexual and reproductive health commodities to survey, including an array of medicines, vitamins, minerals and devices recommended by the WHO and United Nations.
In the coming months, data collectors across the three countries will visit healthcare facilities to survey the price and availability of each selected commodity. They will also conduct brief interviews with healthcare facility representatives to determine what they believe to be the key challenges to providing sexual and reproductive health commodities to patients, as well as ways to improve access. Representatives will also be asked if clients are reluctant to access sexual and reproductive health commodities and, if so, how the taboo can be tackled.
The results of the study will be used by HAI and civil society organisations throughout Kenya, Uganda and Zambia to advocate for better access to sexual and reproductive health commodities in-country and internationally at various global fora. Gemma and the data collectors will likely repeat the survey every year to determine if commodity prices, availability and affordability improve.
“Data on the affordability, availability and access to healthcare services, alone, can’t improve access to sexual and reproductive health commodities, but it’s a necessary first step to understanding the current situation and barriers,” explains Gemma. “Once this evidence is gathered, all healthcare stakeholders—governments, civil society, the WHO, health professionals, industry and others—must work together to develop solutions that improve access. That’s what we’re working towards.”
HAI’s research is being conducted as part of its role on the Health Systems Advocacy (HSA) Partnership, an initiative launched in 2016 with Amref Flying Doctors/Amref Health Africa, the African Centre for Global Health and Social Transformation (ACHEST), Wemos and the Dutch Ministry for Foreign Trade and Development Cooperation. Together, the partners will contribute to the building of stronger health systems so people in sub-Saharan Africa can equitably access high-quality sexual and reproductive health services.
More information on the HSA Partnership is available in this fact sheet.