Theo P.G.M. de Vries, Milan C. Richir, Jelle Tichelaar | 2012 | Download PDF
Introduction
This chapter is intended for medical students and clinical teachers who are interested in learning and/or teaching rational prescribing. In particular, we discuss the WHO Guide to Good Prescribing, which provides an attractive and effective 6-step methodology. We first discuss why the Guide was written and then describe and evaluate the 6-step concept. We conclude with some remarks for therapeutic teachers and medical students.
Why the WHO Guide to Good Prescribing was written
In many medical curricula, teaching in the clinical disciplines is focused on symptoms and diagnosis, and little or no time is given to the principles of drug treatment. Unfortunately many medical schools still provide only short courses or lectures in pharmacotherapy and implicit teaching during clinical clerkships and internships, consisting of rather dogmatic indications of what drug should be used when. This approach goes a long way to explaining why many medical graduates feel insufficiently prepared to assume prescribing responsibilities after graduation, and the many hospital admissions and even deaths caused by possibly avoidable medication errors (Han & Maxwell, 2006; Shelden, 2006). This situation has been pictured in an editorial of the British Journal of Clinical Pharmacology (see figure 1) (Ramsay, 1993).
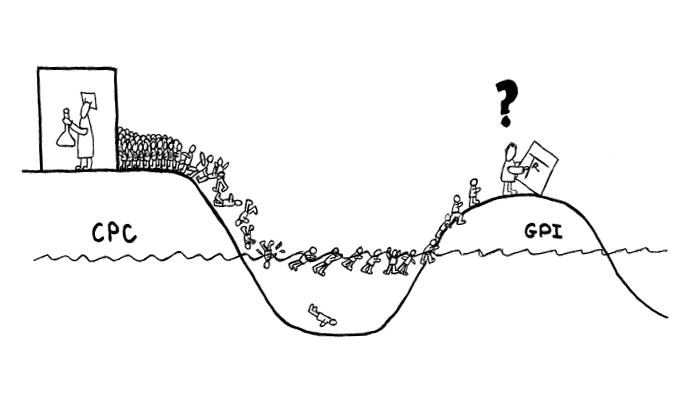
Fig. 1 An impression of the situation of teaching pharmacotherapy. On the left the clinical pharmacology professor on his Clinical Pharmacology Continent (CPC) is beavering away at his research, quite oblivious to what is happening on the General Practice Island (GPI) where most of the drugs are prescribed. Because of his research the clinical pharmacology professor is also not aware of the increasing number of students trying in vain to get his attention in order to be taught therapeutics. The students are seen struggling across the gap towards the real world of medical practice, ill prepared for the task facing them, and some don’t make it (Ramsay, 1993).
It is generally known that attempts to prevent these errors by means of postgraduate training and continuing education programmes for practising doctors have proved disappointing, in particular in the long term. Therefore many doctors have been left to the persuasive methods of the pharmaceutical industry (Wolff, 1970).
In the last 20 years, several initiatives have been taken to improve the undergraduate teaching of pharmacology, clinical pharmacology, and pharmacotherapy, with an emphasis on increasing therapeutic knowledge and skills, often in the preclinical phase (Richir et al., 2008a). However, besides knowledge and skills, future doctors also need to learn in a structured way how to apply their knowledge and prescribing skills in practice, for example, during clinical clerkships and internships, so as to prescribe rationally.
To facilitate the teaching of rational prescribing, the WHO Action Programme on Essential Drugs developed, in collaboration with the University of Groningen, a manual for undergraduate medical students that gives the principles of rational prescribing, the so-called Guide to Good Prescribing (GGP) (de Vries, 1995a). This guide consists of a 6-step model that was originally based on the findings of an unpublished observational study from 1984 involving general practitioners and clinicians in the Netherlands, and on 10 years of experience with pharmacotherapy courses for medical students in some Dutch medical faculties and abroad.
The concept of the WHO Guide to Good Prescribing
The manual presents medical students with a normative model for therapeutic reasoning and prescribing, in the form of a 6-step model of rational prescribing (Table 1).
Step 1: Define the patient’s problem
Step 2: Specify the therapeutic objective
Step 3a: Choose your standard treatment (P-drug)
Step 3b: Verify the suitability of your treatment (P-drug)
Step 4: Start treatment
Step 5: Give information, instructions, and warnings
Step 6: Monitor (and stop?) treatment
Table 1. WHO 6-step model of rational prescribing (de Vries et al., 1995a).
The first step is to define the patient’s problem, to generate a clear indication for treatment. It is in essence a summary of the diagnostic part of the consultation, including complaints, symptoms, and/or diagnosis, and relevant patient characteristics (e.g., comorbidity, co-medication, pregnancy, and drug allergy). In other words, this step forms the basis for choosing and prescribing the correct treatment during the next steps.
The second step is to specify the therapeutic objective, which is essential not only for determining the right treatment, but also for monitoring the effect of treatment later on (step 6). Without clearly specified therapeutic objectives, preferably expressed in measurable parameters, it is not possible to adequately monitor treatment, which could result in incorrect conclusions and further actions.
The third step is to choose which drug or treatment is needed. One of the key principles of the WHO approach is to divide step 3 into two parts: first selection of the so-called p-drug, the prescriber’s Personal drug of first choice for the indication (step 3a), and then confirmation of its suitability for the patient in question (step 3b). Undergraduate students should define their own p-drugs and are encouraged to develop a personal formulary of such drugs during their clinical attachments. These so-called standard treatments should preferably be evidence based.
Verifying the suitability of a p-drug for an individual patient requires thoroughly checking for potential contraindications and for interactions if the patient has co morbidity, is taking other medications, is pregnant, or is allergic to certain drugs etc. Once an appropriate drug has been chosen for the patient in question, it needs to be administered correctly. This involves writing the prescription and starting treatment (step 4), giving the patient information, instructions, and warnings about the treatment (step 5), and monitoring the effect of treatment (step 6). The latter step includes decisions about whether to continue, adjust, or stop the treatment.
In fact, the six steps describe therapeutic skills, and together these skills can be considered to reflect therapeutic competence. Three types of skills can be distinguished: cognitive, communicative, and motor skills (see table 2).
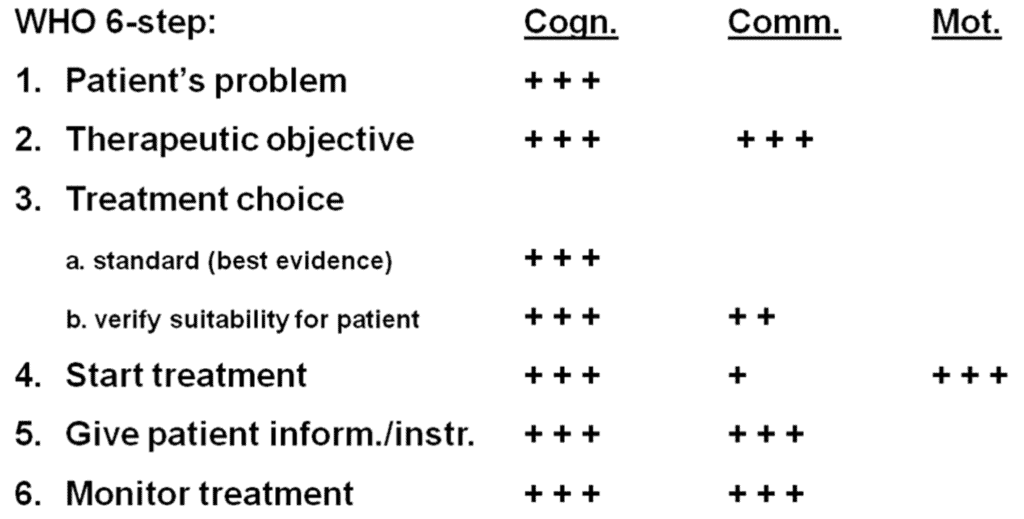
Table 2. The cognitive, communicative and motor skills needed for performing the WHO 6-step
Examples of these skills are selecting the treatment, giving the patient information and instructions, and injecting the drug, respectively. However, as the table shows, some steps consist of two or even three types of skills. All six steps require cognitive skills. Determining the patients’ problem (the indication for the treatment) obviously requires cognitive skills. The same goes for determining the therapeutic objective, but this step also requires communicative skills because the treatment objective should preferably be determined in collaboration with the patient. In the same way, choosing treatment also involves cognitive and communicative skills. Writing a prescription or injecting a drug require knowledge of how to prescribe and how to inject (cognitive), but also the motor skills to administer the drug. Similarly, doctors not only need to determine whát information they should give the patient (and what not!), but also be able to communicate this information to the patient in such a way that the patient can understand what he/she is being told, which increases the chance that treatment will be carried out correctly. Lastly, in the same way, monitoring treatment requires doctors to determine how the treatment should be monitored (cognitive) and an effective way to communicate this to the patient (communicative).
The evaluation of the WHO Guide to Good Prescribing
The Guide has been evaluated in several studies, including a systematic review, as has its impact on clinical teaching. As mentioned in the Introduction, the six-step concept of the Guide was based on an unpublished observational study carried out in 1984 at the University of Groningen in the Netherlands. To our knowledge, this was the first attempt to investigatetherapeutic problem solving by doctors in real practice. Over 500 patient consultations by 25 general practitioners and 25 clinical specialists were observed and recorded, and doctors were interviewed about their therapeutic reasoning. From this study, it became evident that therapeutic problem solving consists of six steps. The study also showed that doctors generally based their choice of drug treatment on two steps. In the first step, doctors used treatment guidelines or drug formularies as a starting point, followed by the second step in which they verified the suitability of this treatment for the individual patient and modified their choice, if necessary (for example, in case of comorbidity or co-medication). Moreover, it was also observed that experienced doctors knew more standard treatments by heart than their less-experienced colleagues.
Several years later, Denig described the process of how therapeutic decisions are made in practice in greater detail (Denig, 1994; Denig, 1992). This study indicated that when a doctor makes a diagnosis, he or she immediately thinks of a number of pharmacotherapeutic possibilities, referred to as the ‘evoked set’. Depending on the diagnosis, the ‘evoked set’ consists of 1.7 to 5 different pharmacotherapeutic options. Although how the final choice of treatment is made for an individual patient is not yet known, it is thought to be either ‘unreasoned’ (routine) or ‘reasoned’ (evaluation of the different options). To a certain extent the results of this study confirmed the findings of the preciously described observational study.
A review of the literature on diagnostic and therapeutic thinking has also confirmed this concept of how drugs are chosen (Figure 2) (Bissessur et al., 2009).
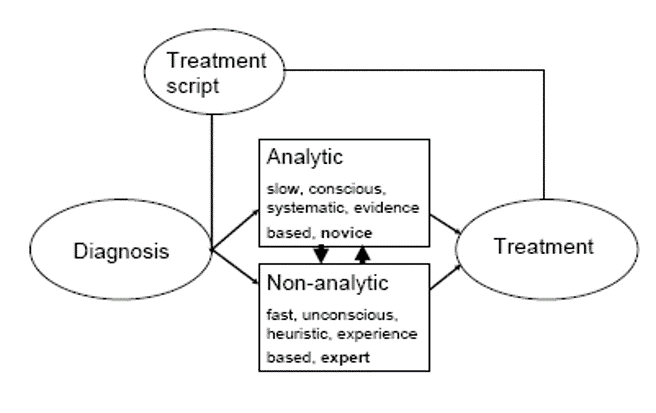
Figure 2: Hypothetical model of therapeutic reasoning (Bissessur et al., 2009).
It showed that, based on the similarities between therapeutic and diagnostic reasoning, it is possible to construct a hypothetical model of therapeutic reasoning. Once the diagnosis has been determined, one or more treatment scripts will be called up from memory. Then an analytical or non-analytical process, or a combination of both, will start, to establish the correct choice of treatment. This process is similar to the process of diagnostic reasoning. The chosen treatment and its effect will contribute to the modification of the existing treatment scripts in the memory, or may result in a new treatment script.
The six-step concept was introduced in a problem-based manner into the curriculum of the University of Groningen en subsequently evaluated (de Vries, 1993a-d). The results of the intervention study were promising, which led to the decision to develop a Guide for students and doctors in collaboration with the WHO. Before publication, the Guide was extensively evaluated and revised by 60 experts from 30 countries.
After publication, studies were performed to measure its impact on students’ and general practitioners’ prescribing (Hassan et al, 2000; Richir et al., 2008b; Vollebregt et al., 2005; Vollebregt et al., 2006; de Vries et al., 1995b; de Vries et al., 2008; Akici, 2003; Akici et al., 2004). These studies showed that the Guide had a positive short-term and long-term effect on the prescribing process. For example, one controlled study evaluated the Guide among 219 undergraduate medical students from six countries (de Vries et al., 1995b). The undergraduate students who used the Guide performed significantly better than the students who did not use the Guide. Not only did students remember how to solve old problems, which had been taught previously, but they could also apply their skills to solve new problems, a so-called transfer effect.
A recent systematic review of these intervention studies showed that, despite some methodological flaws, the 6-step model is the only model that is widely used and which has been shown to improve prescribing (Ross & Loke, 2009). Unfortunately, it remains to be determined whether it affects prescribing in real life, after students have graduated. This will probably prove difficult to determine, because so many other factors influence prescribing that it will be difficult to ascribe any effect solely to the Guide.
The impact of the Guide on clinical teaching has also been evaluated by means of a questionnaire completed by 90 clinical specialists and clinical pharmacology teachers (out of a total of 233) who had been trained by the WHO in Groningen and later at several places in the world in the use of the guide for teaching purposes at medical schools (Smith et al., 2005). The results showed that 75–85% of the respondents used the Guide when teaching drug prescribing, 70% used problem-based teaching methods, and 51% used role–play teaching methods. This high percentage is also partly due to the availability of a Teachers’ Guide to Good Prescribing, which was written at the request of clinical teachers to help them incorporate and implement the Guide effectively in their curriculum (Henning et al., 2001).
Lastly, an indirect indicator of the value of the Guide is the number of languages it has been translated into. As far as we know, the Guide has been translated into around 30 languages. It may be more, because the WHO does not put restrictions on the translation and copying of the Guide.
Final remarks for students and clinical teachers
The WHO Guide to Good Prescribing and the WHO Teachers’ Guide are effective tools for learning and teaching how to prescribe drugs effectively and safely, in a patient-friendly manner, and at reasonable cost. Clinical teachers may find it interesting to read an article on the current status of teaching pharmacotherapy, which includes information about designing a curriculum for teaching in this field (Richir et al., 2008a).
A recent development regarding teaching is the construction of a computer program (P-scribe) according to the 6-step approach by several universities in the Netherlands and Belgium, which is similar to the one used in Australia (van Doorn, 2009; National Prescribing Service Limited, 2010). Another development is the implementation of a practical version of the WHO 6-step into the clinical patient record at the VU University medical center of Amsterdam, in the Netherlands. The therapeutic part of the patient records will be pre-structured by printing the six steps in a practical way so doctors are reminded to write down the essential information regarding the treatment (de Vries, 2009).
Training/examination session of a therapeutic consultation in the outpatient clinic of the VU University Medical Center with a preclinical student in the role of doctor (left), a simulation patient (middle) and a clinician as observer/examiner (right).
All six steps are important – they should be learned and implemented in practice when treating patients. However, based on a remark of one of our students made about 10 years after graduating, one step is crucial and should become part of the genes of each student and medical practitioner. She said: “I loved your teaching, but I must admit that I forgot all the details. However, every time I start to write out a prescription, a red light flashes in my mind, reminding me to check for contraindications and interactions”. We could not have dared to hope that the Guide would have such a beneficial long-term effect on prescribing.
References
Akici, A. (2003). Impact of a short postgraduate course in rational pharmacotherapy for general practitioners. British Journal of Clinical Pharmacology, 57(3), 310-321.
Akici, A. et al. (2004). Comparison of rational pharmacotherapy decision-making competence of general practitioners with intern doctors. European Journal of Clinical Pharmacology, 60, 75-82
Bissessur, S.W. et al. (2009). Therapeutic reasoning: from hiatus to hypothetical model. Journal of Evaluation in Clinical Practice 15, 985-989.
Denig, P. & Haaijer-Ruskamp, F.M. (1992). Therapeutic decision making of physicians. Pharmaceutisch weekblad 14, 9-15.
Denig, P. (1994). Drug choice in medical practice. Thesis, University of Groningen.
van Doorn, A.B.D. et al. (2009). A National Multicentre E-Learning Programme to Promote Cooperation and to Support Rational Prescribing by Future Physicians and Pharmacists. Basic & Clinical Pharmacology & Toxicology 105, 40.
Han, W.H., Maxwell, S.R.J. (2006). Are medical students adequately trained to prescribe at the point of graduation? Views of first year foundation doctors. Scott. Med. J. 51, 27-32.
Hassan, N.A., Abdulla, A.A., Bakathir, H.A., Al-Amoodi, A.A., Aklan, A.M., Vries, Th.P.G.M. de. (2000). The impact of problem-based pharmacotherapy training on the competence of rational prescribing of Yemen undergraduate students. Eur J Clin Pharmacol 55, 873-876.
Henning, R.H., Hogerzeil, H.V., Kosabasoglu, Y.E., Smith, A.J., Summers, R. & Vries, T.P.G.M. de. (2001). Teacher’s Guide to Good Prescribing. Geneva, WHO.
National Prescribing Service Limited. (2010). National Prescribing Curriculum. Available at: http://nps.unisa.edu.au/NPSStart/index.htm [Retrieved March 18, 2010]
Ramsay, L.E. (1993). Bridging the Gap Between Clinical-Pharmacology and Rational Drug Prescribing. British Journal of Clinical Pharmacology 35, 575-576).
Richir, M.C., Tichelaar, J., Geijteman, E.C.T., Vries Th.P.G.M. de. (2008a). Teaching clinical pharmacology and therapeutics with an emphasis on the therapeutic reasoning of undergraduate medical students. Eur J Clin Pharmacol 64, 217-224.
Richir MC et al. (2008b). A Context-Learning Pharmacotherapy Program for Preclinical Medical Students Leads to More Rational Drug Prescribing During Their Clinical Clerkship in Internal Medicine. Clinical Pharmacology & Therapeutics 84, 513-516.
Ross, S. & Loke, Y.L. (2009). Do educational interventions improve prescribing by medical students and junior doctors? A systematic review. Br J Clin Pharamacol 67(6), 662-670.
Sheldon, T. (2006). Dutch doctors call for action on drug safety. BMJ 333, 1238.
Smith, A.J., Hill, S., Walkom, E. (2005). An evaluation of the World Health Organization problem-based pharmacotherapy theaching courses (based on the “Guide to Good Prescribing”), 1994-2001. Eur J Clin Pharmacol 61, 785-786.
Vollebregt, J.A., Metz, J.C., De Haan, M., Hugtenburg, J.G., Vries, Th.P.G.M. de. (2005). Curriculum development in pharmacotherapy: testing the ability of preclinical medical students to learn therapeutic problem solving in a randomized controlled trial. Br J Clin Pharmacol 61, 345-351.
Vollebregt, J.A. et al. (2006). Evaluation of a pharmacotherapy context-learning programme for preclinical medical students. Br J Clin Pharmacol 62, 666-672.
Vries, Th.P.G.M. de. (1993a). Presenting clinical pharmacology and therapeutics: evaluation of a problem based approach for choosing drug treatments. Br J Clin Pharmacol 35, 591-597.
Vries, Th.P.G.M. de. (1993b). Presenting clinical pharmacology and therapeutics: the course in pharmacotherapeutics. Br J Clin Pharmacol 35, 587-590.
Vries, Th.P.G.M. de. (1993c). Presenting clinical pharmacology and therapeutics: a problem based approach for choosing and prescribing drugs. Br J Clin Pharmacol 35, 581-586.
Vries, Th.P.G.M. de. (1993d). Presenting clinical pharmacology and therapeutics: general introduction. Br J Clin Pharmacol 35, 577-579.
Vries, Th.P.G.M. de, Henning, R.H., Hogerzei,l H.V., Fresle, D.A. (1995a) Guide to Good Prescribing. Geneva, World Health Organization.
Vries, Th.P.G.M. de et al. (1995b) Impact of a short course in pharmacotherapy for undergraduate medical students: an international randomized controlled study. Lancet 346, 1454-1457.
Vries, Th.P.G.M. de et al. (2008). Should medical students learn to develop a personal fomulary? Eur J Clin Pharmacol 64, 641-646.
Vries, T.P.G.M. de. (2009). Training Competent Prescribers: Use of A Prestructured Therapeutic Section in the Medical Record. Basic & Clinical Pharmacology & Toxicology, 105, 19.
Wolff, F. (1970). Clinical Pharmacology Yesterday, Today, and Tomorrow. Chest 57, 172-175.
Authors
Theo P.G.M. de Vries, Milan C. Richir, Jelle Tichelaar
Department of Clinical Pharmacology and Pharmacy, section Pharmacotherapy, VU University Medical Center (VUMC), Amsterdam, The Netherlands
Correspondence to:
Professor Th.P.G.M de Vries, MD, PhD
Dept. Clin. Pharmacol. & Pharmacy
VUMC
De Boelelaan 1117
1081 HV Amsterdam
The Netherlands
Phone: +31 (0)20 4448090
Fax: +31 (0)20 4448100
E-mail: thpgm.devries@vumc.nl